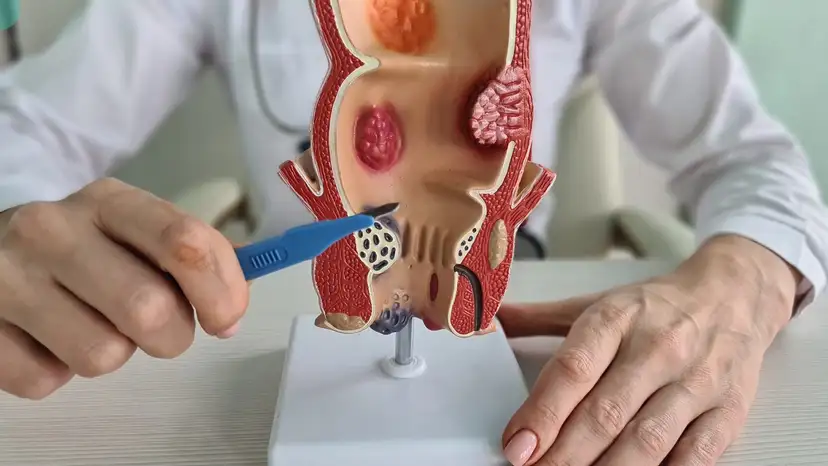
Anal fistulas are small tunnels that form between the end of the bowel and the skin near the anus. They often develop after an abscess in the anal glands fails to heal completely, leaving a persistent infection path. Patients may notice symptoms such as pain, swelling, discharge, or irritation around the anal area. Some experience difficulty with bowel movements, especially if the fistula is complex or located near the sphincter muscles. Chronic inflammation or conditions like Crohn’s disease can also increase the risk of developing an anal fistula. Early detection is crucial to prevent further complications, including recurrent infections or tissue damage. Understanding the nature of fistulas helps patients make informed decisions about treatment options.
Diagnosing an anal fistula involves a combination of clinical evaluation and imaging studies. A physical examination allows the doctor to identify external openings, track inflammation, and assess tenderness. Imaging tests such as MRI or endoanal ultrasound are often used to map the fistula’s pathway accurately. Fistulography, a type of contrast study, can help visualize the entire tract if the path is complex. Proper diagnosis ensures the chosen surgical method addresses all affected areas, reducing the chance of recurrence. Doctors also assess the patient’s overall health, history of abscesses, and bowel habits to tailor the treatment plan. Accurate mapping is particularly important for fistulas that involve the sphincter muscles, as preserving continence is a top priority.
Treatment for anal fistulas may start with non-surgical measures, especially for minor or recently developed cases. These approaches include antibiotics to manage infection, proper hygiene, and sitz baths to reduce discomfort. While these measures can alleviate symptoms temporarily, they rarely eliminate the fistula completely. Persistent or complex fistulas usually require surgical intervention to repair and remove the tract. The primary goals of surgery are to eliminate the infection, promote proper healing, and prevent recurrence. Surgical options are chosen based on the fistula’s location, complexity, and patient factors such as age and overall health. Consulting a colorectal specialist ensures a personalized and effective treatment plan.
Fistulotomy is one of the most commonly performed surgeries for anal fistulas. It involves cutting open the fistula tract to allow it to heal from the inside out. This procedure is typically suitable for simple fistulas that do not pass through a significant portion of the sphincter muscles. Preoperative preparation includes fasting, bowel cleansing, and discussing anesthesia options with the surgeon. During the procedure, the surgeon carefully opens the tract, removes infected tissue, and ensures proper drainage. Postoperative care focuses on pain management, wound cleaning, and maintaining hygiene to prevent reinfection. Healing time varies depending on the fistula’s size, but most patients notice significant improvement within a few weeks. Fistulotomy offers high success rates with a relatively low risk of complications, although minor incontinence may occur in rare cases.
Fistulectomy is another surgical option that involves completely excising the fistula tract. This approach is often recommended for complex or recurrent fistulas, particularly those that extend deeper or involve multiple branches. During a fistulectomy, the surgeon removes the entire tract and surrounding scar tissue while taking care to preserve the sphincter muscles. Imaging studies are essential to ensure no portion of the fistula is left behind, reducing the likelihood of recurrence. Recovery involves careful wound care, pain management, and monitoring for infection. Patients may experience a longer healing period compared to fistulotomy due to the more extensive tissue removal. The procedure’s main advantage is its thoroughness, which minimizes the risk of the fistula returning, although there is a slightly higher risk of temporary incontinence.
Comparing fistulotomy and fistulectomy helps patients understand which method might be best for their condition. Fistulotomy generally offers a shorter recovery period and is less invasive, making it ideal for simple fistulas. Fistulectomy, while more invasive, provides a more complete removal and is often preferred for complex cases. The choice depends on factors such as fistula type, location, prior surgeries, and overall health. Surgeons also consider the patient’s lifestyle and the importance of continence when recommending the procedure. Both methods require careful postoperative care and regular follow-ups to ensure proper healing. Discussing all available options with a colorectal specialist ensures an informed decision and a tailored treatment plan.
Post-surgery, lifestyle adjustments play a critical role in preventing recurrence and promoting healing. Maintaining a high-fiber diet supports regular bowel movements and reduces straining during defecation. Proper hygiene, including gentle cleaning and sitz baths, helps prevent infection and irritation around the surgical site. Patients are advised to avoid prolonged sitting or heavy lifting in the initial recovery period. Regular exercise, once approved by the surgeon, supports overall health and circulation. Monitoring for warning signs such as increased pain, discharge, or swelling ensures timely medical attention if complications arise. These measures, combined with adherence to postoperative instructions, significantly improve long-term outcomes.
- Tips for Supporting Recovery After Anal Fistula Surgery
- Keep the wound clean and dry
- Use prescribed pain medication and antibiotics as directed
- Perform gentle sitz baths multiple times a day
- Maintain a fiber-rich diet to prevent constipation
- Avoid heavy lifting or straining
- Attend all scheduled follow-up appointments
- Watch for signs of infection or unusual discharge
Frequently Asked Questions
- How long does it take to heal after a fistulotomy or fistulectomy?
Healing can take anywhere from four to eight weeks, depending on the procedure and fistula complexity. Patients may experience discomfort during the initial weeks but gradual improvement is expected. - Is there a risk of incontinence after surgery?
Minor temporary incontinence may occur in some cases, especially with complex fistulas. Most patients regain normal bowel control after healing and proper care. - Can anal fistulas recur after surgery?
Recurrence is possible, particularly if the fistula tract was not fully removed or if underlying conditions like Crohn’s disease are present. Proper surgical planning minimizes this risk. - How painful is the recovery process?
Pain varies depending on the surgery type and patient sensitivity. Pain management strategies, including medications and sitz baths, help control discomfort. - Are there alternatives if surgery is not possible?
Non-surgical options, such as antibiotics or seton placement, may manage symptoms but usually do not eliminate the fistula. Surgery remains the definitive treatment for complete removal. - How soon can normal activities resume after repair?
Light activities may resume within a few days, but strenuous exercise or heavy lifting should be avoided until the surgeon confirms adequate healing. Full recovery typically occurs within several weeks.
Takeaway
Anal fistula repair and removal using fistulotomy or fistulectomy provides effective solutions for persistent and complex fistulas. Understanding each procedure, its recovery process, and postoperative care empowers patients to make informed choices and achieve better outcomes. With proper medical guidance and lifestyle adjustments, healing is manageable, and the risk of recurrence can be significantly reduced.